Waking up multiple times during the night to urinate, also known as nocturia, is a common yet disruptive condition that affects millions of people worldwide. It is different from bedwetting, as those with nocturia are usually able to get up and walk to the bathroom on their own. However, the frequent interruptions in sleep caused by nocturia due to excessive urination at night can significantly impact quality of life. In this article, we will discuss the various causes, its different types, and available treatment options.
What is Nocturia?
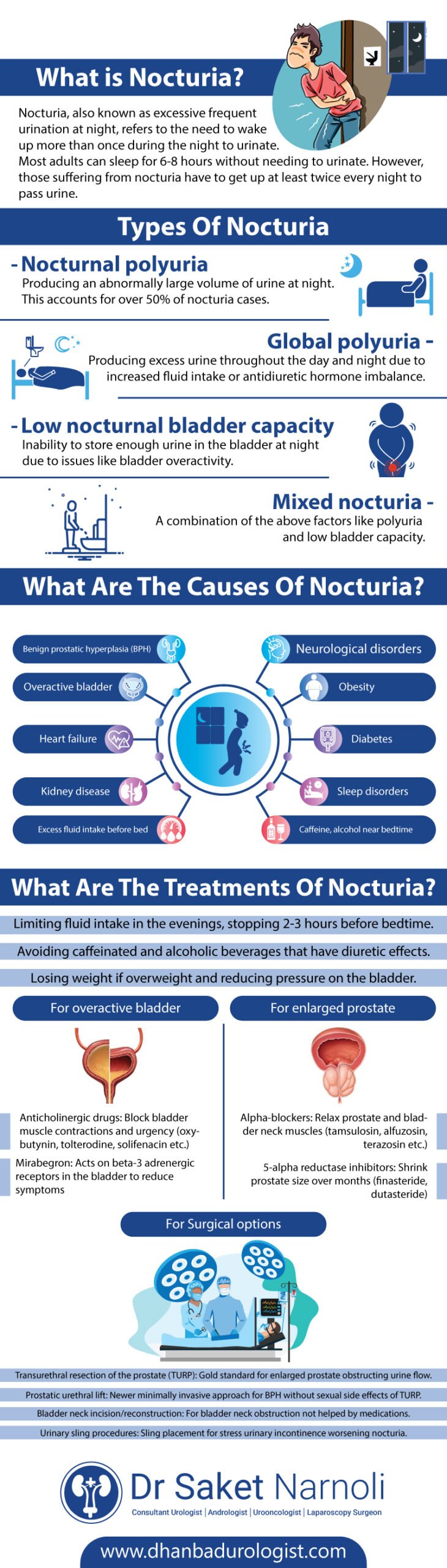
Nocturia, also known as excessive frequent urination at night, refers to the need to wake up more than once during the night to urinate. Most adults can sleep for 6-8 hours without needing to urinate. However, those suffering from nocturia have to get up at least twice every night to pass urine.
Nocturia is a common condition, especially among older adults. Studies show that nearly 1 in 3 adults over the age of 30 experience nocturia, waking up at least twice every night to urinate. The frequency and severity of nocturia tend to increase with age. While occasional nocturia may be normal, frequent or long-standing episodes could indicate an underlying medical problem.
Types of Nocturia
Nocturia has different causes and types depending on what is driving the excessive nighttime urination. The main types include:
- Nocturnal polyuria: Producing an abnormally large volume of urine at night. This accounts for over 50% of nocturia cases.
- Global polyuria: Producing excess urine throughout the day and night due to increased fluid intake or antidiuretic hormone imbalance.
- Low nocturnal bladder capacity: Inability to store enough urine in the bladder at night due to issues like bladder overactivity.
- Mixed nocturia: A combination of the above factors like polyuria and low bladder capacity.
Understanding the type of nocturia helps doctors determine the appropriate evaluation and treatment.
What are the Causes of Nocturia?
A variety of medical conditions and lifestyle factors can potentially cause or contribute to nocturia causes. Some of the most common causes include:
Medical Conditions
- Overactive bladder (OAB): Bladder muscle spasms and urgency to urinate frequently at night.
- Benign prostatic hyperplasia (BPH): Enlarged prostate pressing on the urethra in men causing urinary issues.
- Heart failure: Fluid retention in the body from poor cardiac function.
- Kidney disease: Impaired ability of kidneys to concentrate urine at night.
- Diabetes: Frequent urination due to high blood sugars or diabetic nephropathy.
- Neurological disorders: Conditions affecting bladder control like Parkinson’s disease.
- Sleep disorders: Conditions like sleep apnea disrupting normal sleep patterns.
Lifestyle Factors
- Excess fluid intake before bed: Drinking too much liquid in the evenings.
- Caffeine, alcohol near bedtime: Diuretic beverages close to sleep time.
- Obesity: Extra weight putting pressure on the bladder.
- Medications: Diuretics and other drugs linked to nocturia as a side effect.
- Pregnancy: Hormonal changes and pressure on the bladder from the uterus.
Identifying and addressing underlying causes is a key part of nocturia treatment. Lifestyle modifications are often the first approach tried before considering medical therapies.
Evaluating Nocturia
A doctor will perform a thorough evaluation for anyone experiencing frequent nighttime urination. This typically involves:
- Medical history: Questions about symptoms, onset, associated conditions, medications, fluid intake etc.
- Physical exam: Checking for issues like prostate enlargement in men.
- Urinalysis: Testing a urine sample for signs of infection.
- Bladder diary: Recording fluid intake and urination patterns over 3-4 days.
- Nocturia severity index: Questionnaire scoring symptom impact on quality of life.
- Special tests: As needed, like cystoscopy, ultrasound, urodynamic testing or sleep studies.
The goal is to identify underlying causes, assess nocturia severity, and rule out other conditions. This guides determining the best treatment approach.
Lifestyle and Behavioral Treatments
Making lifestyle modifications is usually the first line approach for their treatment before considering medications:
- Limiting fluid intake in the evenings, stopping 2-3 hours before bedtime.
- Avoiding caffeinated and alcoholic beverages that have diuretic effects.
- Losing weight if overweight and reducing pressure on the bladder.
- Good bladder habits like not delaying urination and emptying the bladder before sleep.
- Raising the head of the bed by 6 inches to reduce fluid pooling in the legs and pelvis.
- Wearing compression stockings to minimize leg swelling in those with circulatory issues.
- Treating any underlying sleep disorders like sleep apnea that disrupt sleep.
- Timed naps and leg elevation during the day to reduce fluid urinary retention.
- Lifestyle changes can provide relief for many nocturia sufferers when adhered to consistently.
Medication Therapies
When lifestyle modifications prove insufficient, drug therapy may be needed. Medications are tailored based on the underlying cause:
For overactive bladder (OAB)
- Anticholinergic drugs: Block bladder muscle contractions and urgency (oxybutynin, tolterodine, solifenacin etc.)
- Mirabegron: Acts on beta-3 adrenergic receptors in the bladder to reduce symptoms
For enlarged prostate (BPH)
- Alpha-blockers: Relax prostate and bladder neck muscles (tamsulosin, alfuzosin, terazosin etc.)
- 5-alpha reductase inhibitors: Shrink prostate size over months (finasteride, dutasteride)
Other causes
- Desmopressin: Synthetic antidiuretic hormone used in diabetes insipidus, enuresis, etc.
- Diuretics: Used cautiously in some cases under medical guidance.
- Medications provide relief in about 50-60% of cases but side effects must be weighed against benefits. Combination drug therapy may also be tried in refractory cases.
Surgical Options
When all conservative options fail, surgery to address the underlying structural cause may be recommended:
- Transurethral resection of the prostate (TURP): Gold standard for enlarged prostate obstructing urine flow.
- Prostatic urethral lift: Newer minimally invasive approach for BPH without sexual side effects of TURP.
- Bladder neck incision/reconstruction: For bladder neck obstruction not helped by medications.
- Urinary sling procedures: Sling placement for stress urinary incontinence worsening nocturia.
While highly effective, surgery involves more risks than minimally invasive options. It is only considered after exhausting behavioural and drug therapies.
Alternative and Herbal Remedies
Some alternative therapies may provide relief for nocturia linked to overactive bladder, but evidence is limited:
- Cranberry juice: May help prevent urinary tract infections worsening nocturia.
- Acupuncture: Short-term relief reported but needs more research.
- Herbal supplements like pumpkin seed oil extract, raspberry leaf, and stinging nettle root.
Always consult a doctor before trying alternatives, as safety and interactions with medications are unknown. Lifestyle changes and prescription therapies remain the mainstay of their treatment.
Conclusion
Nocturia can significantly impact quality of life when severe or long-standing. A thorough evaluation helps identify causes and tailor treatment. Lifestyle modifications should always be attempted first with medications and minimally invasive options considered for persistent symptoms. Surgery is a last resort option for structural issues not helped by other means. If you are also seeking medical help for urological issues , you can contact and book an appointment with Dr.Saket Narnoli , who is known to be the Best Urologist in Dhanbad Providing Excellent Urological Services. With a tailored treatment plan and lifestyle modifications, urinary retention can usually be managed successfully. With a stepwise treatment approach and patient compliance, nocturia can usually be managed successfully.






